Breathing Through the Butt: A Scientist’s Unexpected Journey to Revolutionize Oxygen Delivery
When Dr. Takanori Takebe watched his father struggle with pneumonia and undergo the invasive process of being placed on a ventilator, it sparked a question that would lead him down an unusual research path: Could humans possibly breathe through their rectums? This seemingly bizarre inquiry has evolved into serious scientific research with potentially life-saving applications.
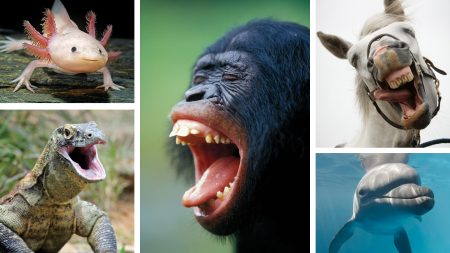
Dr. Takebe, who divides his time between Cincinnati Children’s Hospital Medical Center and the University of Osaka, normally focuses on developing lab-created livers to treat organ failure. However, his concern about his father’s respiratory treatment—especially given his dad’s previous partial lung removal—pushed him to explore alternative methods of delivering oxygen to the human body. The inspiration for his unconventional approach came from nature, after a graduate student brought him a book describing how various animals obtain oxygen through different body parts. Certain freshwater fish called loaches, for instance, can swallow air to supplement their gill breathing when oxygen levels in water are low. With his background in gastroenterology, Takebe recognized that the human intestinal tract, rich in blood vessels (which is why certain medications can be delivered via enemas), might potentially serve as an entry point for oxygen delivery.
This insight led Takebe and his team to develop an innovative treatment using perfluorodecalin, a liquid already employed in various medical procedures. This special liquid can carry oxygen and, crucially, also absorb carbon dioxide—essentially mimicking the gas exchange function of lungs. Their initial experiments with mice and pigs yielded promising results: enemas containing this oxygen-rich liquid helped the animals survive low-oxygen conditions. In pigs, each 400-milliliter dose boosted blood oxygen levels for approximately 19 minutes, with later tests showing improvements lasting up to half an hour. Takebe vividly recalls watching samples of pig blood transform from a muddy, low-oxygen color to a brighter, oxygen-rich red—a transformative moment that convinced him they were onto something significant. The unconventional nature of the research earned Takebe’s team an Ig Nobel Prize in 2024—an award celebrating science that first makes people laugh, then think—where Takebe playfully accepted the honor wearing a loach-shaped hat while thanking the audience “for believing in the potential of the anus.”
Moving from animal studies to human trials, Takebe’s team recently tested the safety of their approach in 27 healthy male volunteers in Japan. Each participant received a dose of non-oxygenated perfluorodecalin administered rectally and was asked to retain it for an hour. The doses ranged from a minimal 25 milliliters to a substantial 1.5 liters (the maximum approved amount for contrast agents used in GI tract X-rays). While four of the six men in the highest-dose group had to stop treatment early due to stomach pain, those receiving up to 1 liter generally tolerated the procedure well, experiencing only mild discomfort and bloating. These findings, published in the December 2022 issue of Med, represent an important step forward, though the research—funded by EVA Therapeutics, a startup co-founded by Takebe—still has a long way to go.
The scientific community remains divided on the potential of “butt breathing.” Dr. John Laffey, a specialist in acute respiratory distress syndrome at the University of Galway, expresses significant skepticism. He argues that researchers should focus on improving treatments that support the lungs rather than recruiting other body parts to perform lung functions. Laffey points out practical limitations: “A liter of perfluorodecalin carries 500 milliliters of oxygen. We use 250 milliliters per minute…. A back-of-the-envelope calculation here would tell you it’s just very hard to see how this would work.” The need for repeated, frequent enemas to maintain oxygen support presents a significant challenge to the approach’s practicality.
On the other hand, Dr. Kevin Gibbs, a pulmonary critical care physician at Wake Forest University, sees potential value in the concept despite initial surprise. He notes that during the critical procedure of intubating patients for ventilator support—which can expose them to dangerously low oxygen levels for several minutes—a quick oxygen boost through this alternative method could prove invaluable. “What I find exciting is if this drug works… maybe you can administer this, and then all of the sudden they have this real boost in oxygen for the time it takes you to safely put someone on life support—and that would be huge.” Takebe similarly envisions intestinal oxygen delivery as a supplement to conventional breathing support or as a short-term emergency measure when other treatments aren’t immediately available, such as during hospital transfers or ambulance transport.
As for the inspiration behind this unusual research direction—Takebe’s father—he remains enthusiastic about his son’s work. “Dad is pleased,” Takebe reports with a smile, noting that his father has even offered to serve as an experimental subject, though ethical considerations would prevent such participation. Nevertheless, Takebe values his father’s encouragement as he continues to explore this unconventional but potentially life-saving approach to oxygen delivery—one that reminds us that medical innovation sometimes comes from thinking about old problems from completely new angles.