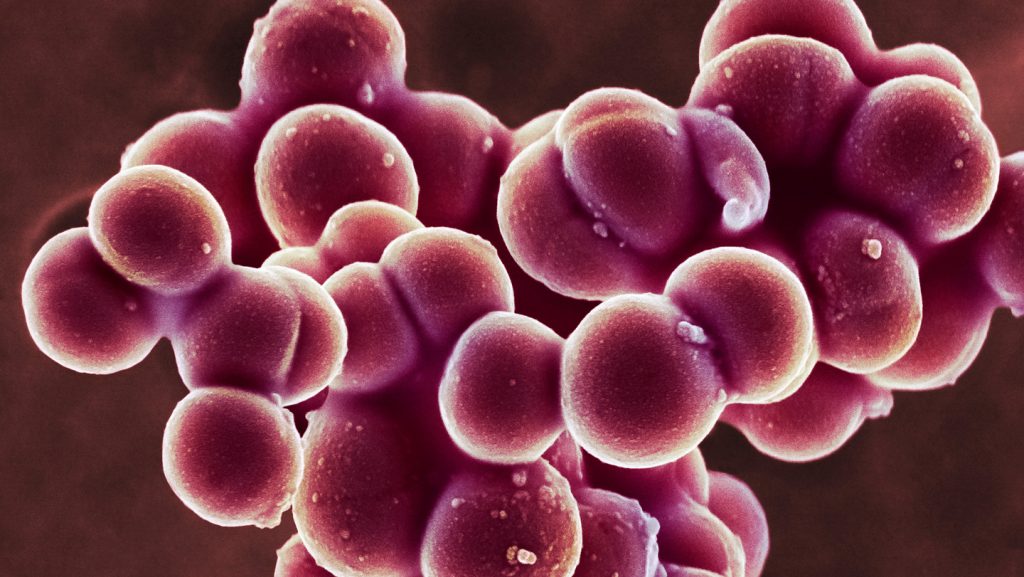
The Remarkable Tenacity of Skin Bacteria: Understanding Staph’s Powerful Grip
When it comes to microscopic tenacity, few organisms can match the impressive staying power of Staphylococcus aureus. Recent research published in the September 5 issue of Science Advances reveals that this common bacterial culprit behind staph infections possesses one of the strongest biological bonds ever documented in nature. The way these tiny organisms cling to human skin isn’t just impressive—it’s nearly unbreakable, especially when strengthened by calcium, preventing these bacterial cells from being easily washed or brushed away.
The significance of this discovery extends beyond mere scientific curiosity. “The mechanism that we use to fix a bruise is the same mechanism that the bacteria take advantage of to bind better to our skin,” explains Rafael Bernardi, a biophysicist at Auburn University in Alabama. When skin becomes damaged—whether through a minor cut or a condition like eczema—the body releases calcium to accelerate healing and skin regeneration. Unfortunately, this natural healing response creates the perfect environment for S. aureus to establish its remarkably strong grip.
Through sophisticated microscopy and computer simulations, Bernardi and his colleagues conducted a detailed analysis of the molecular interaction between two key proteins: SdrD from the bacteria and DSG-1 from human skin. Their findings were astounding. When calcium is present, these proteins forge a bond capable of withstanding forces stronger than 2 nanonewtons—a strength virtually unprecedented in biological systems without a covalent bond (where atoms share electrons). To put this in perspective, most mechanical forces within cells measure in piconewtons (a thousandth of a nanonewton), with even muscle contraction proteins breaking apart at around 60-80 piconewtons. The bacterial grip is approximately 20 times stronger than these muscular forces, leading Bernardi to observe that at the molecular level, these tiny bacteria “can grip more stronger than your muscles can lift.”
This remarkable adhesion ability has profound implications for human health. S. aureus can transform from a harmless skin resident to a dangerous pathogen when it invades the body through breaks in the skin, potentially causing infections ranging from localized skin conditions like cellulitis to life-threatening systemic infections when the bacteria spread to other organs. The bacterium’s extraordinary binding capability is a key factor in this disease progression, as it enables the organism to establish a secure foothold before beginning its invasion.
While different strains of staph commonly inhabit human skin, researchers are still investigating whether binding strength varies among these strains. Regardless, the findings open promising avenues for new treatment approaches. Some antibiotic-resistant varieties of staph, such as MRSA (Methicillin-resistant Staphylococcus aureus), form protective biofilms—slimy shields surrounding bacterial clusters that make infections particularly difficult to treat. Bernardi suggests that if we could prevent the initial attachment of individual bacterial cells to skin by disrupting the SdrD-DSG-1 interaction, biofilm formation might be prevented entirely, allowing immune cells or antibiotics to effectively eliminate the bacteria.
This research marks a significant step forward in our understanding of bacterial adhesion mechanisms and could potentially lead to the development of novel therapeutic approaches that don’t rely on traditional antibiotics. By targeting the fundamental attachment process rather than attempting to kill bacteria that have already established themselves, scientists may discover new ways to combat even the most stubborn staph infections, including those resistant to conventional treatments.