The Double-Edged Sword of Mast Cells: A Deep Dive into Nexocytosis and Allergic Inflammation
The human immune system is a complex and dynamic network of cells and molecules that work together to protect the body from harmful invaders. Within this intricate system, mast cells play a crucial role as sentinels, constantly patrolling the tissues and initiating inflammatory responses upon encountering foreign substances. While this inflammatory response is essential for combating infections and repairing damaged tissues, it can also go awry, leading to allergic reactions and other immune-related disorders. Recent research has uncovered a surprising new mechanism by which mast cells contribute to allergic inflammation, a process termed "nexocytosis." This intricate interplay between mast cells and another type of immune cell, neutrophils, sheds new light on the complexities of the immune response and may pave the way for novel therapeutic approaches to managing allergic conditions.
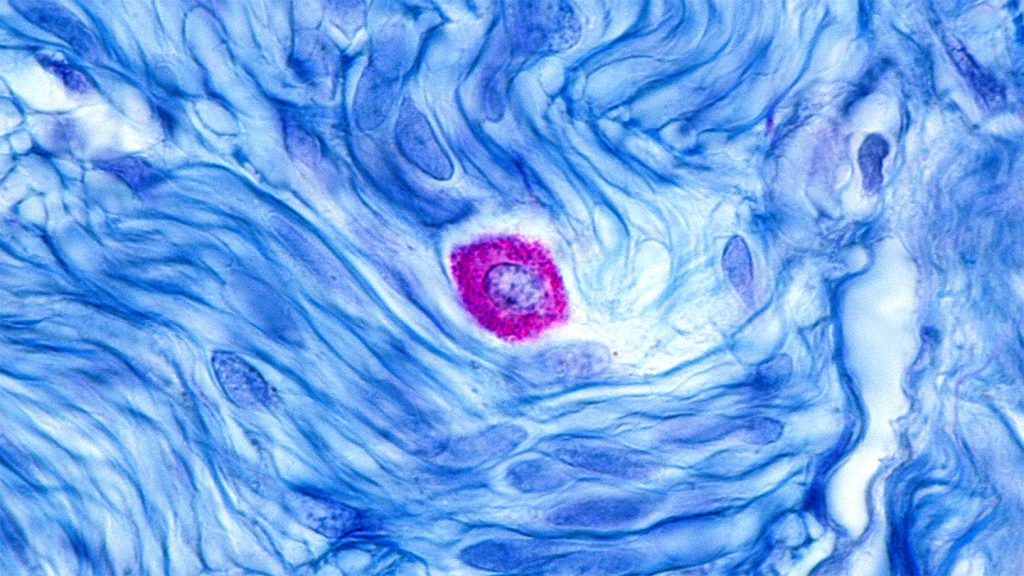
Mast cells are strategically located throughout the body, particularly in tissues that come into contact with the external environment, such as the skin, lungs, and gastrointestinal tract. These cells are equipped with granules, small sacs filled with potent inflammatory mediators like histamine and heparin. Upon encountering an allergen, a typically harmless foreign protein, mast cells become activated and release their granule contents, triggering the characteristic symptoms of an allergic reaction, including itching, swelling, and redness. Traditionally, this degranulation process was considered the primary mechanism by which mast cells contributed to allergic inflammation. However, recent findings have revealed a more complex and nuanced role for these immune sentinels.
A team of researchers, led by immunologist and biochemist Michael Mihlan, made a startling discovery while investigating the interactions between mast cells and neutrophils. Neutrophils are another type of immune cell, belonging to a class of white blood cells called granulocytes. They are among the first responders to sites of infection or injury, playing a critical role in eliminating pathogens and clearing cellular debris. Mihlan and his colleagues observed that, in addition to releasing their granule contents, activated mast cells also attract and engulf neutrophils in a process akin to phagocytosis, the cellular "eating" of foreign particles. This unexpected finding challenged the existing understanding of mast cell function and highlighted a previously unknown level of interaction between these two key immune players.
The researchers, using both mouse and human cells, observed a fascinating sequence of events. Activated mast cells released chemical signals that attracted neutrophils to their location. Once in close proximity, the mast cells proceeded to engulf the neutrophils, effectively trapping them within their cellular confines. This phenomenon was observed in response to exposure to a human blood protein, suggesting that the process could be triggered by a variety of stimuli. Even more surprisingly, the researchers found that even after the trapped neutrophils died within the mast cells, their remnants, including proteins, DNA, and other molecules, persisted within the mast cell. These cellular leftovers could then be utilized by the mast cell for its own sustenance or packaged and expelled during subsequent allergic reactions, a process the researchers dubbed "nexocytosis."
Nexocytosis represents a novel mechanism by which mast cells contribute to allergic inflammation. By capturing and then expelling the contents of neutrophils, mast cells effectively amplify and perpetuate the inflammatory response. This process has significant implications for understanding the underlying mechanisms of allergic diseases like asthma and dermatitis, characterized by chronic inflammation and tissue damage. The persistence of neutrophil remnants within mast cells raises the possibility that these cells may serve as a reservoir of inflammatory mediators, contributing to the long-term effects of allergic reactions. Furthermore, the discovery of nexocytosis suggests that interventions targeting the interaction between mast cells and neutrophils could offer new therapeutic avenues for managing allergic conditions.
While the role of nexocytosis in allergic inflammation is now becoming clearer, further research is needed to fully elucidate its implications and potential therapeutic applications. Mihlan and his team are actively investigating whether this process may also have beneficial effects in certain contexts, such as fighting off bacterial infections. It is plausible that the capture and subsequent expulsion of neutrophils by mast cells could serve as a mechanism for enhancing the immune response against pathogens. This possibility highlights the dual nature of the immune system, capable of both protective and destructive actions depending on the specific circumstances.
The intricate dance between mast cells and neutrophils, as revealed by the discovery of nexocytosis, provides a deeper understanding of the complex interplay between different components of the immune system. This new insight into the mechanisms of allergic inflammation opens doors to developing more targeted and effective treatments for allergic diseases. As researchers continue to explore the multifaceted roles of mast cells and their interactions with other immune cells, we can anticipate further advances in our understanding and management of allergic conditions, ultimately improving the lives of millions affected by these debilitating disorders.