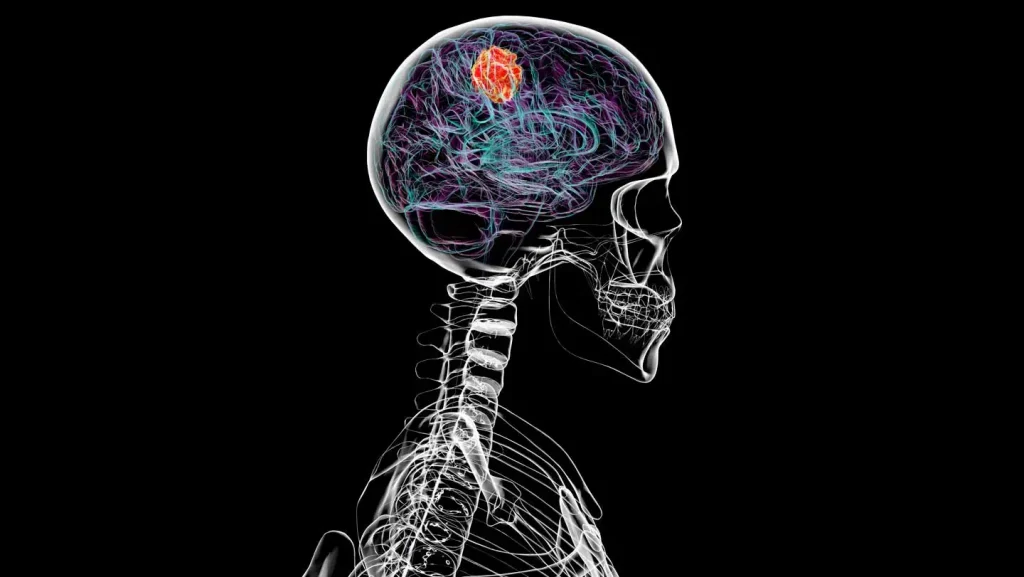
Glioblastoma’s Far-Reaching Impact Beyond the Brain
Glioblastoma, the most aggressive form of primary brain cancer, has long been studied for its devastating effects on brain tissue. However, recent research has uncovered a more extensive pattern of damage that extends beyond the neural environment. This formidable cancer doesn’t confine its destruction to brain matter alone; it systematically alters surrounding structures, particularly the protective skull that houses our most vital organ. Scientists have discovered that glioblastoma actively erodes bone tissue in the skull, creating a previously unrecognized pathway of destruction. Even more concerning, the cancer appears to infiltrate the bone marrow within the skull, fundamentally changing the composition of immune cells that reside there. These discoveries point to glioblastoma as a more systemically invasive disease than previously understood, with tendrils of influence that reach beyond the blood-brain barrier into the very framework that supports and protects the brain.
The bone deterioration caused by glioblastoma represents a significant and overlooked aspect of the disease progression. As tumor cells proliferate within the brain, they release signals that activate bone-destroying cells called osteoclasts in the surrounding skull. This leads to thinning and weakening of the bone structure—a process similar to osteoporosis but localized and accelerated by the cancer’s presence. Imaging studies of glioblastoma patients have revealed concerning patterns of bone density loss in areas adjacent to tumor sites, sometimes creating almost imperceptible channels through which cancer cells might potentially escape the cranial cavity. This bone erosion doesn’t typically cause obvious symptoms distinct from the neurological effects of the tumor itself, which may explain why it remained largely undetected until researchers specifically looked for these changes. Understanding this bone deterioration could provide new avenues for monitoring disease progression and potentially developing interventions that preserve skull integrity.
Perhaps even more profound than the structural changes to the skull is glioblastoma’s remarkable ability to reshape the immune environment within skull bone marrow. The marrow spaces within cranial bones house specialized immune cells that differ somewhat from those found in long bones throughout the body. When glioblastoma establishes itself in the brain, it appears to send chemical signals that fundamentally alter the development and function of these nearby immune cells. Researchers have documented shifts in the populations of immune cells, with increases in certain types that actually suppress immune responses against cancer while decreasing those that might otherwise attack tumor cells. This manipulation of the nearby immune system essentially creates a protective shield for the cancer, training the body’s defense mechanisms to ignore or even support the tumor’s growth rather than fighting against it. This subversion of immune function may help explain why glioblastoma so effectively resists many treatment approaches.
The discoveries about glioblastoma’s effects on both bone structure and immune function have important implications for treatment approaches. Current standard therapies, including surgery, radiation, and chemotherapy, focus almost exclusively on targeting the tumor within brain tissue. However, if the cancer is simultaneously creating a supportive environment in surrounding structures, these approaches may be missing critical aspects of the disease. Future treatments might need to address not only the primary tumor but also the bone deterioration and immune dysfunction it causes. This could involve combining traditional brain cancer therapies with medications that strengthen bone (similar to those used for osteoporosis) and immunotherapies specifically designed to reverse the cancer’s manipulation of skull marrow immune cells. Some researchers are already exploring whether certain bone-preserving drugs might improve outcomes for glioblastoma patients, not just by preventing fractures but by potentially interfering with the cancer’s ability to spread or evade immune detection.
These findings also shed new light on why glioblastoma has proven so resistant to treatment over decades of research efforts. The brain tumor microenvironment has always been recognized as complex, but adding bone interaction and immune subversion to this picture creates an even more challenging therapeutic target. The cancer appears to create multiple layers of defense—from the blood-brain barrier that blocks many drugs, to the reprogrammed immune cells that should be attacking it, to the altered bone structure that potentially provides new pathways for tumor expansion. This multi-faceted approach to self-preservation makes glioblastoma particularly resilient against single-target treatments. The interconnected nature of these systems suggests that effective therapies may need to simultaneously address multiple aspects of the disease rather than focusing on killing tumor cells alone. This helps explain why even aggressive surgical removal of visible tumor tissue so often fails to prevent recurrence.
For patients and families affected by glioblastoma, this expanded understanding of the disease offers both challenges and hope. On one hand, recognizing the cancer’s ability to affect systems beyond the brain underscores its formidable nature and helps explain the difficulties faced in treatment. On the other hand, each new discovery about how glioblastoma operates opens potential avenues for intervention that weren’t previously considered. Researchers are now investigating whether blood tests that detect bone turnover markers might help monitor disease progression, potentially catching recurrence earlier than brain scans alone. Others are exploring whether immune cells harvested from areas away from the skull marrow might be more effective for immunotherapy approaches. While glioblastoma remains one of medicine’s most difficult challenges, this broader perspective on how it affects the entire cranial environment—brain, bone, and immune system together—may ultimately lead to more comprehensive and effective treatment strategies that address the full scope of this devastating disease.