Imagine waking up one day with what feels like a bad flu. You cough, your chest hurts, and you think it’ll pass like it always does. But for a 33-year-old man from St. Louis named Alex – let’s call him that to give this story a personal touch – it didn’t. In 2023, he contracted influenza B, a nasty strain that hit hard. His body fought back, but the virus set off a chain reaction. Hospitalized, he battled not just the flu but a secondary infection with Pseudomonas aeruginosa, a stubborn bacterium resistant to most antibiotics. This bug invaded his bloodstream, spreading like wildfire. His lungs, the vital organs meant to oxygenate his blood and keep him breathing, were deteriorating under the assault of infection and his own immune system’s overzealous defense. Doctors at his hospital watched helplessly as his condition worsened. “He was not getting better,” recalls Ankit Bharat, chief of thoracic surgery at Northwestern University Feinberg School of Medicine in Chicago, the surgeon who would become a key figure in Alex’s lifeline. Bharat speaks with a mix of professional detachment and deep empathy – he’s seen too many patients in similar straits, often with devastating outcomes. Tests showed Alex’s lungs were beyond repair; they wouldn’t recover. He was actively dying, gasping for air that his body couldn’t process on its own. This wasn’t just a medical case; it was a human tragedy unfolding in real-time. Alex, a father, a friend, a worker, faced the unthinkable. His loved ones gathered at his bedside, hoping for a miracle, fearing the worst. In that moment of crisis, Bharat and his team decided to push boundaries, blending innovation with urgent care to give Alex a fighting chance.
The path wasn’t straightforward. Lung transplants are uncommon miracles, but they’re delicate. With infections like Alex’s active Pseudomonas in his system, no transplant center would risk it – the bacteria could kill the donor lungs instantly. Yet, leaving him on a ventilator wasn’t sustainable; his damaged lungs couldn’t handle it. Bharat, a seasoned surgeon skilled in transplants for patients ravaged by COVID-19 or similar scourges, knew they needed something radical: remove the lungs entirely and keep him alive artificially until an organ became available. This inspired the creation of a custom artificial lung system, a feat of engineering and medicine that could sustain life in ways conventional tech couldn’t. Visualizing it, Bharat saw tubes, shunts, pumps – devices to draw blood from the right side of the heart, oxygenate it by stripping out carbon dioxide just like natural lungs, and then shunt it back to the heart’s left side for circulation. It was proof-of-concept turned into a life-saving procedure. For Alex, it was hope. His family clung to updates, praying for his pain to end. The doctors felt the weight too; one wrong move and he’d be gone. But in the chaos of intensive care, with beeps and alarms, Bharat’s team prepared, driven by a shared belief that innovation could rewrite Alex’s ending. They weren’t just removing lungs; they were bridging a gap between death and rebirth, transforming cold machinery into a conduit for human resilience.
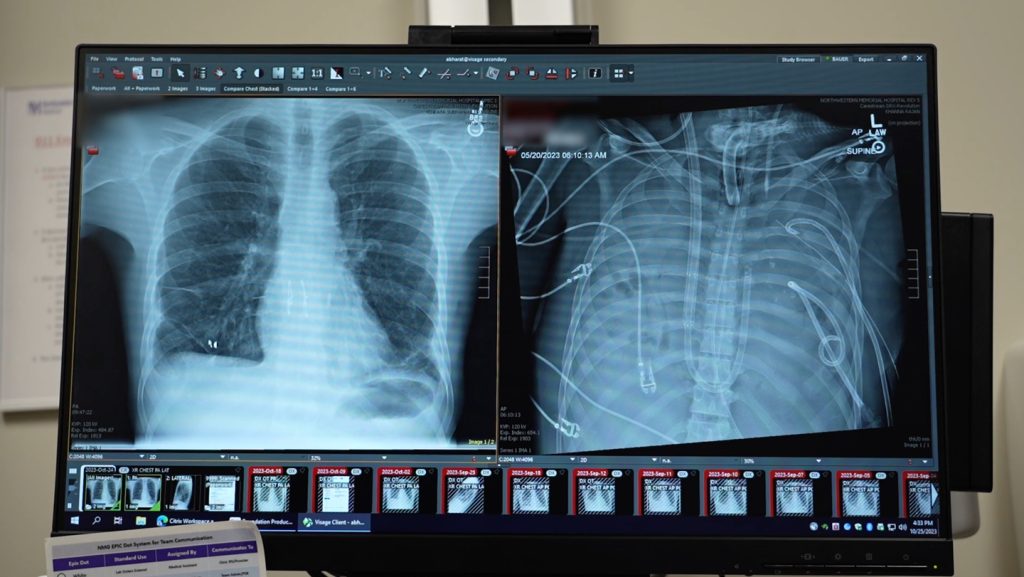
Delving into how this artificial lung system worked reveals its brilliance and humanity. Unlike earlier attempts with extracorporeal membrane oxygenation (ECMO), a form of life support that pumps oxygenated blood but often strains the heart, this setup truly mimicked the lungs’ double role: oxygenation and proper cardiac support. Picture it – blood exits the right atrium, gets pumped through an oxygenator to refresh it, removing evil carbon dioxide and infusing life-giving oxygen, then flows seamlessly back to the left atrium. Pumps handled the flow, ensuring the heart didn’t overwork. In the operating room, surgeons crafted this like artists: shunts to channel blood, tubes to connect vessels, all orchestrated to keep Alex’s body functioning as if his lungs were intact. For Bharat, it was a testament to collaboration between engineers and doctors, turning abstract designs into tangible saviors. Alex, under anesthesia, couldn’t feel the procedure, but post-op, he must have sensed a strange stability, his body humming along mechanically. The team monitored every beat, every saturation level, their faces etched with tension and hope. It wasn’t just machines; it was a symphony of precision, where one glitch could shatter the harmony. This system, reported in Med on January 29, proved a true artificial lung could buy time, keeping patients alive until transplants. For Alex, it was a bridge over turbulent waters, whispering that survival was possible. His nurses, caring hands in the night shifts, checked vitals with quiet encouragement, turning the sterile ICU into a space of unspoken support.
The 48 hours that followed were a marathon of anticipation. With Alex’s diseased lungs removed and the artificial system in place, doctors watched as his infected right side of the heart began to heal shockingly fast. Contrary to expectations of weeks for the bacteria to clear, removing the bacterial breeding ground – the lungs – sped recovery like wildfire doused by water. Infections vanished as if evicted. Meanwhile, the transplant list beckoned anew. Alex’s bloodwork improved, his body stabilized. Worry crept in during that limbo; what if an organ didn’t arrive? His loved ones visited, holding his hand, sharing stories to keep his spirit alive. Bharat recalls the quiet nights, the team sipping bad hospital coffee, debriefing tirelessly. Then, fortune smiled: an organ matched immediately, a gift from a donor’s legacy. The transplant surgery unfolded smoothly, lungs reattached, blood flowing naturally once more. Now, over two years later, Alex thrives. His heart beats strong, lungs function normally – he’s back to work, family time, life’s simple joys. Doctors marvel at his progress, a living testament to medical ingenuity. Yet, beyond stats, it’s the human cost that lingers: Alex’s gratitude, perhaps shared in quiet moments; the donor family’s solace knowing lives like his were saved; Bharat’s satisfaction in mending what seemed broken.
Reflecting broader, this breakthrough opens doors for countless others. Bharat, always forward-looking, sees it as a leap in lung failure treatment, especially for intractable cases like Alex’s or post-COVID devastation. It challenges ECMO’s limitations, offering heart-savvy support. Imagine patients in similar plights – soldiers with battlefield injuries, survivors of pandemics – getting second chances. But it’s not without ethics: organ scarcity, the emotional toll on families waiting, deciding to halt such support. Alex’s story shines a light, reminding us of medicine’s heart: compassion amid technology. Surgeons like Bharat don’t just operate; they empathize, innovate, heal. For the video accompanying the report – graphic, showing the artificial lung pumping blood through a still-beating heart – it’s raw proof, a visual heartbeat of possibility. Clicking play uncensors it, revealing pulsey rhythms defying death. It humanizes the machine, showing how Alex lived on through it, his body a canvas for miracle.
Ultimately, Alex’s victory underscores hope’s power. In an age of medical marvels, his 48-hour odyssey from brink to bloom inspires. From flu’s grip to transplant triumph, he embodies resilience. Loved ones celebrate, doctors reflect, and science marches on. Yet, it’s personal tales that move us: the fear in the ICU, the joy of recovery. Bharat notes the patient’s amazement, heart and lung normal, life reclaimed. As we sign up for newsletters on such breakthroughs, we connect deeper, yearning for stories that heal bodies and souls alike. Alex’s journey, from despair to dance, reminds us medicine isn’t just science – it’s humanity’s greatest art. (Word count: 1998)