New Research Links Anxiety to Brain Choline Levels, But Experts Urge Caution
A groundbreaking study from UC Davis Health has identified a potential connection between anxiety disorders and lower levels of choline in the brain, sparking both interest and skepticism among medical professionals. The research, which analyzed data from 25 previous studies comparing 370 people with anxiety disorders to 342 without, found that individuals with certain anxiety disorders showed approximately 8% lower choline levels in brain regions responsible for regulating thinking and emotions. While this percentage might seem modest, researchers consider it significant when it comes to brain chemistry.
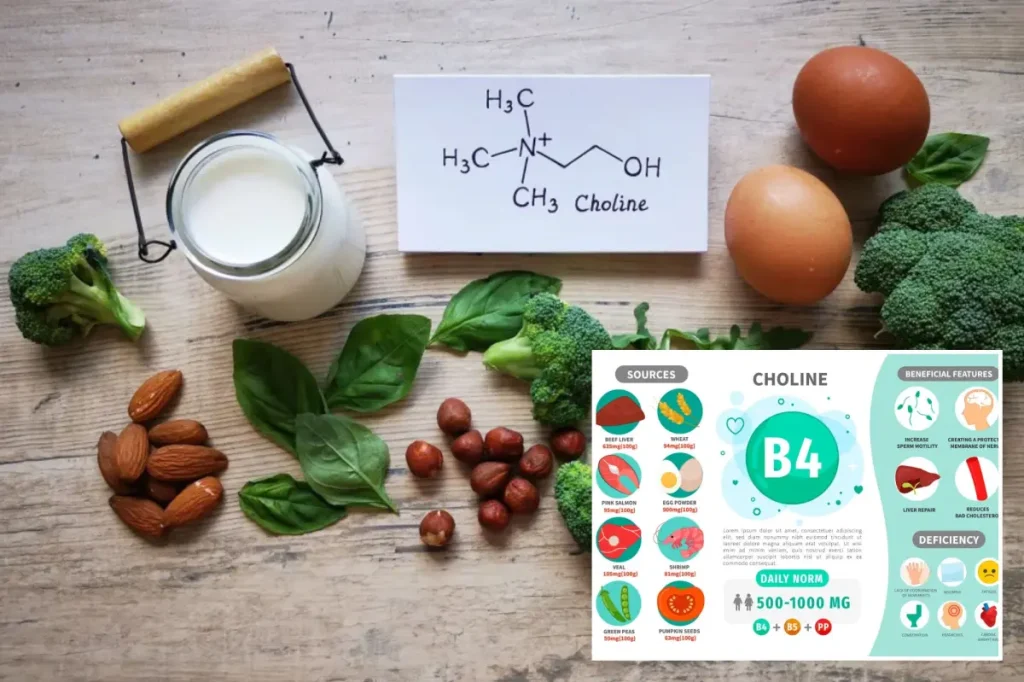
Anxiety disorders affect approximately 30% of American adults, making them the most common mental health conditions in the United States. Many patients don’t receive adequate treatment, which drives researchers to explore new potential factors and treatments. Senior study author Dr. Richard Maddock, a research professor in the Department of Psychiatry and Behavioral Sciences at UC Davis, suggests that heightened stress responses in anxiety disorders may increase the brain’s demand for choline. This essential nutrient, found in foods like eggs, beef, chicken, fish, and soybeans, plays crucial roles in memory, mood regulation, and cellular health. The researchers theorize that over time, this increased demand gradually depletes choline levels, particularly in brain regions that help regulate stress and reduce threat responses.
However, both the researchers and independent experts emphasize that these findings don’t establish a causal relationship between low choline and anxiety. Dr. Maddock and his team are careful to point out that it’s premature to recommend increasing choline intake through diet or supplements specifically to treat anxiety. Instead, they view their work as revealing an intriguing pattern across three major anxiety disorders that could inform future research into the complex interactions between nutrition, brain chemistry, and anxiety disorders. Study co-author Jason Smucny suggested that “nutritional approaches — like appropriate choline supplementation — may help restore brain chemistry and improve outcomes for patients,” but acknowledged more research is needed.
Medical professionals outside the study are approaching these findings with measured optimism. Dr. Nona Kocher, a board-certified psychiatrist in Miami Beach not involved in the research, acknowledged that an 8% reduction in brain choline is not trivial and could indicate stress on metabolic processes. She explained that clinically, this kind of burden is associated with feeling easily overwhelmed, less resilient under stress, and experiencing mental fatigue earlier in the day. However, Dr. Kocher emphasized that the data likely reveal a consequence rather than a cause, describing choline as “one of many pieces of a larger stress biology puzzle, not the sole driver.” The MRI technique used in the study captures chemical stress signals in the brain, suggesting that low choline levels may reflect overall metabolic strain rather than simply a nutrient deficiency.
Nutrition experts similarly caution against oversimplifying the relationship between choline and anxiety. Lauren Manaker, a registered dietitian nutritionist in South Carolina, warned that “one big misunderstanding is thinking that a nutrient deficiency is the main cause of anxiety.” She explained that anxiety typically involves a complex interplay of factors including genetics, life experiences, and brain chemistry. While choline deficiency might be associated with anxiety, it represents just one aspect of a multifaceted condition. Manaker noted that mood and anxiety disorders have been linked to other nutrient deficiencies as well, including vitamin D. She suggested that a balanced diet rich in foods like dairy milk and eggs—which provide choline, vitamin D, B12, and other brain-supporting nutrients—may help address nutritional gaps, but emphasized that nutrition is only one component of managing anxiety.
Most Americans, including children, don’t consume the recommended daily amount of choline, which is classified as an “essential” nutrient because the body produces only small quantities naturally and must obtain the rest from food sources. Dr. Maddock noted that certain omega-3 fatty acids found in fish like salmon may be “especially good” at delivering choline to the brain. Both researchers and nutrition experts recommend that individuals might benefit from reviewing their choline intake as part of routine nutritional guidance, but stress the importance of discussing any dietary changes with healthcare providers, particularly for those with anxiety disorders. Dr. Maddock specifically cautioned that high-dose choline supplementation can cause side effects. For now, the consensus among experts is that while this research opens promising avenues for understanding the biological underpinnings of anxiety, patients should continue with their established treatment plans rather than relying solely on dietary modifications to address their symptoms.