A Fight for Life and Affordability: How Prescription Drug Prices Impact American Patients
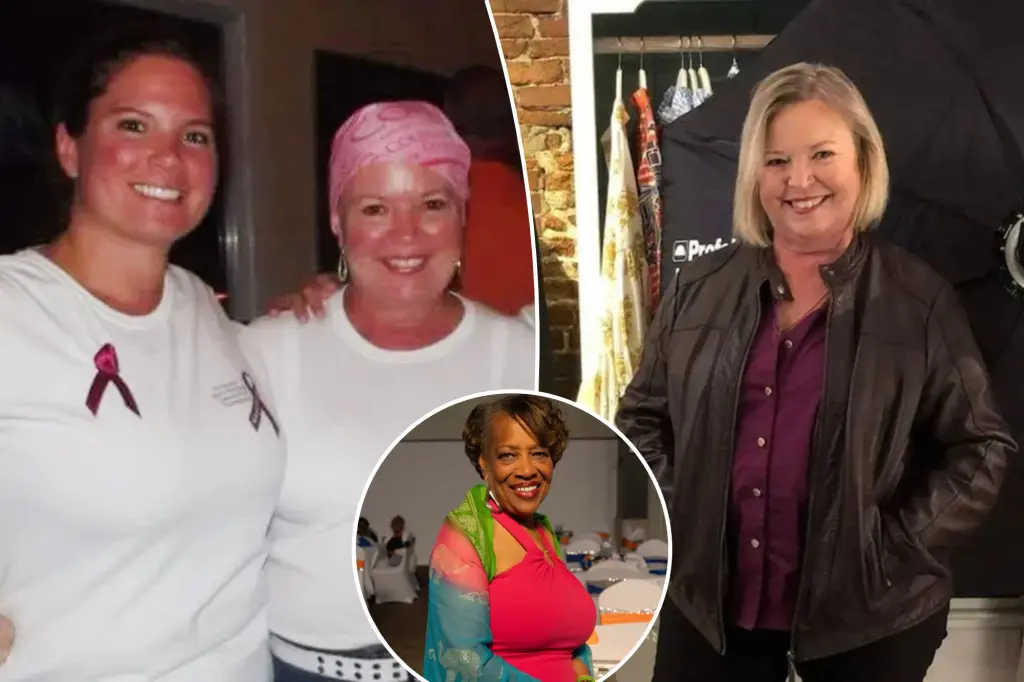
For critical care nurse Janet Kerrigan, the devastating news came in 2011. Diagnosed with multiple myeloma—an incurable blood cancer—she was given just one or two years to live. While a stem cell transplant in 2012 offered hope, it came with an overwhelming financial burden: her private insurance covered only 80% of the nearly million-dollar procedure. Then came the prescription for Revlimid, a vital drug that activates the immune system to fight cancer cells, with a staggering $11,000 co-pay. “This is a drug that’s going to keep my myeloma at rest,” explains Kerrigan, now 69 and living in Myrtle Beach, South Carolina. “It’s like a diabetic needs insulin. Myeloma patients need Revlimid, so I just went into action.” What followed was a desperate scramble—liquidating assets, including her grandmother’s silver, organizing family fundraisers, taking on side jobs, and applying for grants—anything to afford the medication that kept her alive. Her story highlights a crisis facing countless Americans: the prohibitively high cost of prescription drugs that forces patients to choose between financial ruin and their health.
The issue of prescription drug prices recently returned to national attention when President Trump announced new efforts to lower costs. Pfizer agreed to reduce prescription drug costs for Medicaid, and a “TrumpRx” website is being developed to offer discounted medications for uninsured and underinsured Americans. Kerrigan, now retired and on Medicare, sees this as the “beginning of the help that we need.” She believes these changes will eventually create a “trickle-down effect” beyond just Medicaid recipients. The stark reality of American drug pricing becomes clear when Kerrigan notes that she knows myeloma patients who can purchase a three-month supply of their medications for just $80—in India. This disparity is not unique to cancer drugs; Americans pay nearly three times as much for prescription medications as citizens of other high-income nations, highlighting a systemic problem that transcends individual illnesses or drug categories.
Trump’s plan includes pursuing a “most-favored-nation” (MFN) drug pricing framework to align U.S. costs with those of other wealthy countries. Since his September 30 announcement, some pharmaceutical companies have already taken action. AstraZeneca launched AstraZeneca Direct to sell prescribed medications at discounted cash prices, including asthma rescue inhaler Airsupra and diabetes drug Farxiga. Similarly, French drugmaker Sanofi will expand its $35 monthly insulin program to all U.S. patients with valid prescriptions starting in January 2024, regardless of insurance status. While Trump promised savings of up to 85% with his initiative, critics contend these measures may not go far enough for patients to experience meaningful financial relief. For people like Aarolyn McCullough, a 66-year-old retired U.S. Postal Service worker who takes 16 pills daily after receiving a liver transplant, any assistance would make a significant difference in her $600 quarterly medication expenses, which force her to cut back on travel, entertainment, and dining out.
Both Kerrigan and McCullough have channeled their personal struggles into advocacy through Patients for Affordable Drugs, a national organization dedicated to lowering prescription drug prices. Kerrigan had the opportunity to meet with Health and Human Services Secretary Robert F. Kennedy Jr. last summer to advocate for relief. During this meeting, she shared her humiliating experience of having to cash in her grandmother’s silver to pay for medical bills, passionately asserting that “nobody should have to go through this.” Kerrigan felt that Kennedy “really listened” and appeared “very, very empathetic” to their cause, even expressing anger at the obstacles patients face in accessing their medications. Following the meeting, Kennedy stated that reducing prescription drug prices to match those of other nations is “the only humane thing and compassionate thing that we can do for Americans,” suggesting potential support at the highest levels of health policy.
Despite the financial stress of managing their conditions, both women have transformed their experiences into platforms for helping others. McCullough assists transplant patients at Henry Ford Hospital in Detroit, where she received her own liver transplant in 2011. She also runs the nonprofit Aarolyn’s House of Hope, envisioning a supportive space for organ recipients and their families similar to the Ronald McDonald House model. Kerrigan founded a support group for myeloma patients and their caregivers in the Myrtle Beach area, providing emotional support alongside practical advice for navigating the healthcare system. After undergoing a personalized form of immunotherapy in 2023, she is back in remission and currently off prescription medications—a fortunate outcome that many patients never experience.
For Kerrigan, McCullough, and millions of Americans facing similar challenges, the fight for affordable prescription drugs is not just about financial stability—it’s about dignity and the fundamental right to health. “Why should somebody that has cancer have to worry where we’re going to get our drugs in the United States?” Kerrigan asks, highlighting the cruel irony of living in one of the world’s wealthiest nations while being unable to afford life-saving medication. Lower drug prices “would be a lifesaver for a lot of people,” not just in the literal sense of ensuring access to medication, but by relieving the psychological burden that accompanies financial distress. As pharmaceutical companies begin responding to political pressure and policy changes, patients hope that meaningful reform will finally make essential medications accessible to all Americans who need them—regardless of their financial circumstances or insurance status.