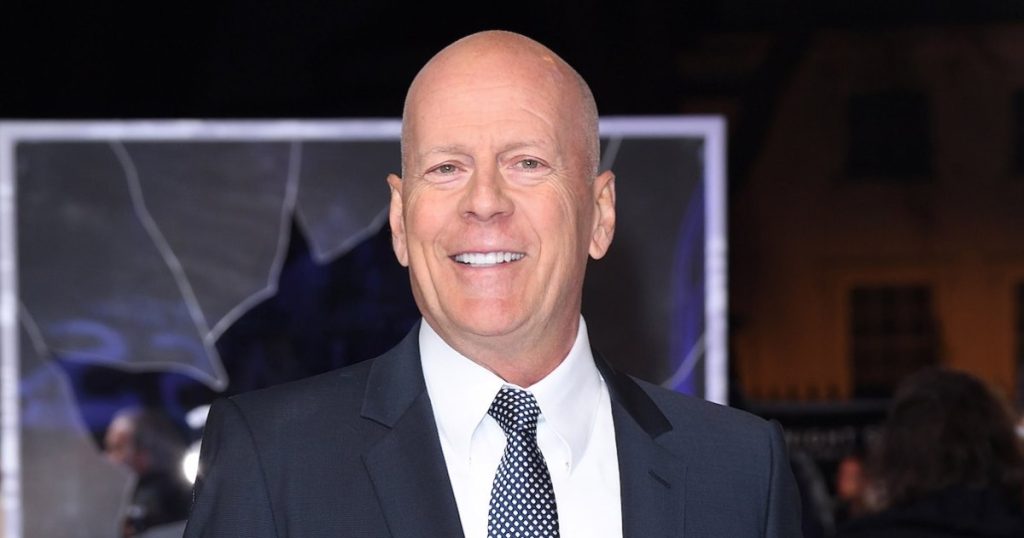
Bruce Willis’s Journey with Dementia: Finding Balance for Family and Care
In a heart-wrenching revelation that resonated with families facing similar challenges, Emma Heming Willis recently shared that her husband, beloved actor Bruce Willis, has moved into a separate home as he battles frontotemporal dementia (FTD). This difficult decision highlights the complex realities many families face when caring for loved ones with progressive neurological conditions. The 70-year-old actor, known for his dynamic roles in films like “Die Hard” and “Pulp Fiction,” now requires full-time specialized care as his condition advances. Emma, who shares daughters Mabel, 13, and Evelyn, 11, with Bruce, described this as “one of the hardest decisions” she’s had to make, underscoring the emotional weight caregivers carry when navigating such life-altering circumstances.
The journey to this arrangement wasn’t simple or straightforward. As Mallory Grivner, a licensed clinical social worker specializing in aging and caregiving issues, explains, “Living arrangements are often dependent on a few factors, including available caregivers, physical setup of the home, the individual’s care needs, goals of care and finances.” For many families, keeping a loved one with dementia in familiar surroundings offers advantages – familiar environments can promote routine and independence while potentially reducing the grief and disorientation that can accompany relocation. However, FTD presents unique challenges that sometimes necessitate specialized environments. Patients with this condition can be particularly sensitive to noise and stimulation, which became increasingly difficult to manage in a household with two young children. Emma revealed that before the move, she had limited her daughters’ social activities, preventing playdates and sleepovers, which led to feelings of isolation for the entire family.
The decision to create separate living spaces ultimately centered around creating environments that served everyone’s needs appropriately. “We have two young children, and it was just important that they had a home that supported their needs and that Bruce could have a place that supported his needs,” Emma explained. This arrangement allows the children to maintain some normalcy – having friends over, enjoying typical childhood activities – while ensuring their father receives the calm, structured environment that best supports his condition. Dr. Kylie Meyer, a gerontologist and assistant professor at Case Western Reserve University, notes that while it’s “not uncommon for persons living with dementia to live in a separate residence than their primary caregiver,” having a second home specifically for this purpose is less common due to financial constraints. The Willis family’s resources have allowed them to create a solution that many families couldn’t access, highlighting disparities in dementia care options based on economic means.
Safety considerations play a paramount role in determining appropriate living arrangements for individuals with dementia. Nancy Treaster, a certified caregiving consultant, emphasizes that home safety is the “first priority” for families, regardless of where the person with dementia resides. “People with dementia often wander and may get into dangerous situations, so families must effectively ‘childproof’ their home for an adult-sized person,” she explains. This can include securing external doors, installing locks on cabinets containing potentially dangerous items, covering stove knobs, and blocking off stairs. For the Willis family, these safety concerns became increasingly difficult to address while also maintaining a suitable environment for two active children. Emma reflected on the decision-making process: “Sometimes it means that you have to look at your house. You have to look at is it safe for someone to be living in this house? Is it safe for me, and is it safe for our children?”
The emotional toll of caregiving rarely receives enough attention in discussions about dementia. Emma candidly shared that she sought treatment for depression while trying to find appropriate care solutions for her husband. This acknowledgment highlights an often-overlooked aspect of the caregiving journey – the immense psychological burden carried by those supporting loved ones with degenerative conditions. Dr. Meyer points out that caregiver wellbeing must be part of the equation when considering living arrangements: “We also must think about the caregiver: how does this living arrangement affect them? Especially with spousal caregivers, many types of dementia can seriously impact their ability to get a good night’s sleep, which is so needed to take care of themselves and the care recipient.” Grivner adds that “caregiving is extremely challenging and taking care of your own needs is important,” addressing the guilt many caregivers feel when they can’t provide all necessary care themselves.
Despite the physical separation, the Willis family remains deeply connected. Emma and the children visit Bruce regularly, maintaining their bond while creating a structure that serves everyone’s needs. “Everything just feels a lot calmer, more at ease now,” Emma shared, though she described the decision as “heartbreaking.” This bittersweet reality reflects the journey of countless families navigating dementia care – finding solutions that balance medical needs with emotional wellbeing for all involved. The Willis family’s openness about their experience has helped illuminate the challenges faced by those caring for loved ones with FTD and other forms of dementia, potentially reducing stigma and encouraging others to seek appropriate support. Their story reminds us that there are no perfect solutions in dementia care, only thoughtful choices made with love, guided by the unique circumstances of each family, and focused on preserving dignity and quality of life for everyone involved.