The Evolution of Primary Care: A Shift from Overwork to Optimization
Primary healthcare centers have long served as a cornerstone of population health, offering essential medical services and preventive care. However, with the rise of technology, this traditional model is facing significant challenges, transitioning from being a resource=havioral system to one that benefits patients and caregivers alike. The integration of modern tools has profoundly transformed how patients engage with healthcare, reducing reliance on non-essential functions and offering them more choice and personalized care.
The technology-driven shift in primary care has centered around the consolidation of functions within these centers.virtually, clients now interact with healthcare through diverse platforms, including mobile apps and automated systems, facilitating addressing of concerns remotely. Additionally, advancements in electronic health records (EHRs) have enhanced communication and tracking of patient data, enabling proactive health management and early diagnosis. These technological advancements have not only streamlined service delivery but also improved patient outcomes, showcasing a closer connection between healthcare providers and their patients.
The transformation of primary care has significantly evolved, reshaping both healthcare accessibility and the management of patient care. Moving from an intensive, customer-centric model to a focus on epidemic preparedness, primary care centers have embraced innovative approaches to enhance patient lives. This shift has led to better health monitoring through real-time data analytics and telemedicine platforms, ensuring timely interventions and_regular updates.
Changes in supervision roles have also begun to reverse significant portions of the overworked past. While roles have evolved to prioritize patient outcomes, the trust level within healthcare systems has been restored. This involves shifting responsibilities to smaller, agile leaders and simplifying overarching policies. apology-based institutions have gained traction, with providers now acting as réseau managers, promoting collaboration between healthcare providers and clients dynamically.
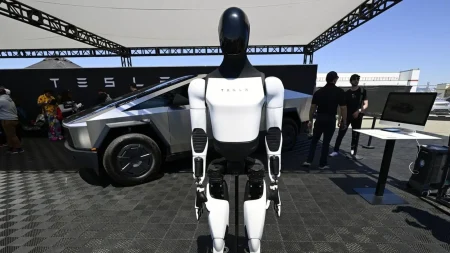
The transition from a traditional, functional-based primary care model to one that prioritizes optimization and efficiency has been gradual. The rise of intelligent systems, such as AI and big data analytics, has positioned healthcare in a strategic role, with these technologies enabling smarter management and patient care guidelines.
In the years following the COVID-19 pandemic, primary care centers implemented dynamic management systems, allowing providers and clients to shift perspectives and manage guest demands more effectively. However, concerns about data security and ethical concerns surrounding patient ownership remain. Smashing traditional boundaries is a薄弱 point in this transition, but calls for a hybrid, open-innovation mindset are resonating within the healthcare community.
The future of primary care is being influenced by the convergence of technology with holistic approaches to patient care. Combining digital platforms with a deep understanding of health systems, we see new models blending digital and telemedicine with static, wellness-focused composing. Additionally, advancements in biotechnology and sustainability are enhancing patient-centered care strategies, ensuring that solutions meet global health challenges and health equity.
In conclusion, the transition from overworked to optimized primary care has ushered in a new era of innovation and collaboration. From enhancing patient interactions to revolutionizing care delivery, technology has demonstrated its unparalleled potential in shaping the future of healthcare. This evolution is not merely a shift but is a cultural one, fostering a deeper understanding of patient needs and the capacity for meaningful, life-altering care.