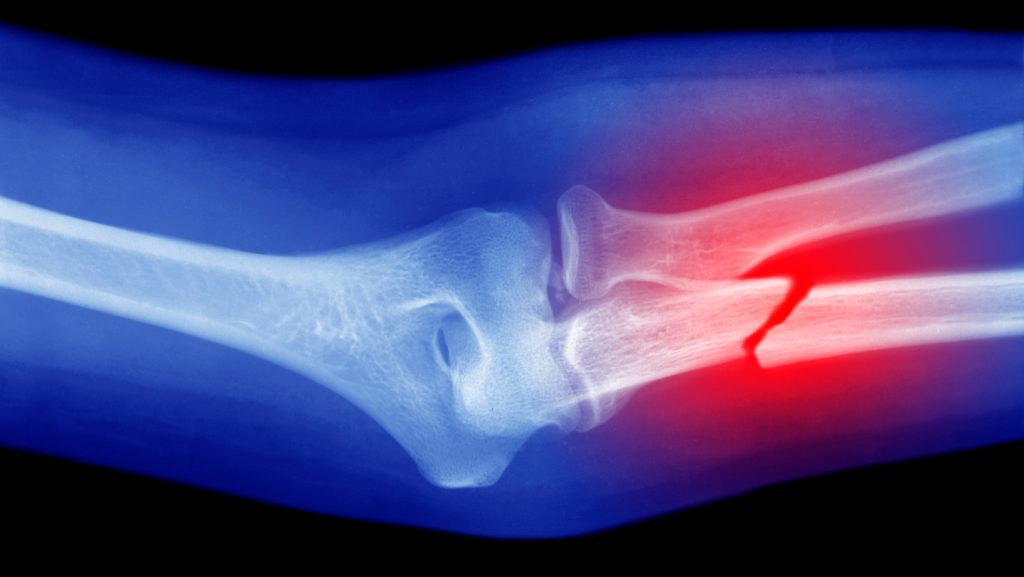
Revolutionary Handheld Device Brings On-the-Spot Bone Grafting to Surgical Settings
In a groundbreaking development that could transform orthopedic surgery, researchers have created a handheld device capable of applying synthetic bone grafts directly at injury sites without the need for prior imaging or complex fabrication. This innovation, reported in the journal Device on September 5, essentially modifies a hot glue gun to 3D print specialized “bioink” directly onto bone fractures. The technology represents a significant departure from conventional methods that typically require time-consuming preparation of custom implants based on detailed scans.
“We can save time, cost and complex procedures compared with those required in conventional 3D printing-based bone graft fabrication,” explains biomedical engineer Jung Seung Lee of Sungkyunkwan University in Seoul, South Korea, who led the research. Traditional approaches to bone grafting involve taking detailed measurements of injuries to build precisely specified implants – a process that can take days and potentially delay crucial surgeries. Lee’s team sought to create a printing system that could be readily equipped and utilized in clinical settings, bringing the benefits of advanced biomaterials directly to the operating room.
The innovative bioink at the heart of this technology combines two compounds with proven track records in implant fabrication: hydroxyapatite and polycaprolactone (PCL). Hydroxyapatite supports bone formation pathways and enhances tissue regeneration, while PCL – a biocompatible plastic approved by the U.S. Food and Drug Administration – creates the scaffold for new bone growth. “PCL gradually degrades in our body over months,” Lee notes. “This enables the slow substitution of the graft with the newly grown bone tissue.” A key advantage of this formulation is its adaptability; the proportions of these compounds can be adjusted to optimize the material’s strength, stiffness, and biochemical properties for specific applications. The researchers also incorporated antibiotics into the bioink to prevent post-surgical infections, enhancing its clinical utility.
The practical application of this technology is remarkably straightforward. The bioink is loaded into the modified printing device and applied directly where needed. Since conventional hot glue guns operate at temperatures that would damage living tissues, the researchers made crucial modifications to restrict heat output and improve control through an adjusted tip design. Thanks to PCL’s low melting point, the bioink can be applied at approximately 60 degrees Celsius and cools to body temperature within 40 seconds. The entire application process takes just minutes, with surgeons able to control the direction, angle, and depth of the device during printing – offering unprecedented flexibility in treating complex bone injuries.
To validate their approach, Lee’s team tested the device on femoral bone fractures in rabbits, comparing results with a control group receiving standard bone cement. The findings were promising: rabbits treated with the bioink showed superior healing and bone tissue regeneration. Importantly, none of the animals exhibited signs of infection during the 12-week post-surgery monitoring period, suggesting the effectiveness of the antibiotic component. These results provide compelling evidence for the potential clinical value of this technology, though Lee emphasizes that it remains a proof of concept at this stage. Before reaching human operating rooms, the technology will require standardized manufacturing processes, sterilization protocols, and further animal studies to ensure safety and efficacy.
Looking ahead, Lee envisions developing this into a multifunctional printing system incorporating additional therapeutic substances such as growth factors and specialized drugs for various orthopedic applications. While the current prototype faces certain limitations – including concerns about the elevated temperature potentially stressing cells, as noted by Deborah Mason, a molecular and cell biologist at Cardiff University – the researchers are actively addressing these challenges by modifying the device tip to accelerate temperature reduction after extrusion. Biomaterials engineer Nieves Cubo-Mateo from Nebrija University in Madrid sees the potential for this technology to evolve into a true “bone printer pen” for surgeons, though she notes significant development remains necessary, particularly in ensuring compatibility with imaging technologies and robotic assistance systems used in modern surgical settings. With continued refinement, this handheld bone grafting device could ultimately become not just a defect-filler but a comprehensive regenerative tool adaptable to different surgical specialties, potentially revolutionizing treatment approaches for millions of patients with bone injuries worldwide.