Rethinking Early Breast Cancer Treatment: Exploring Active Monitoring for DCIS
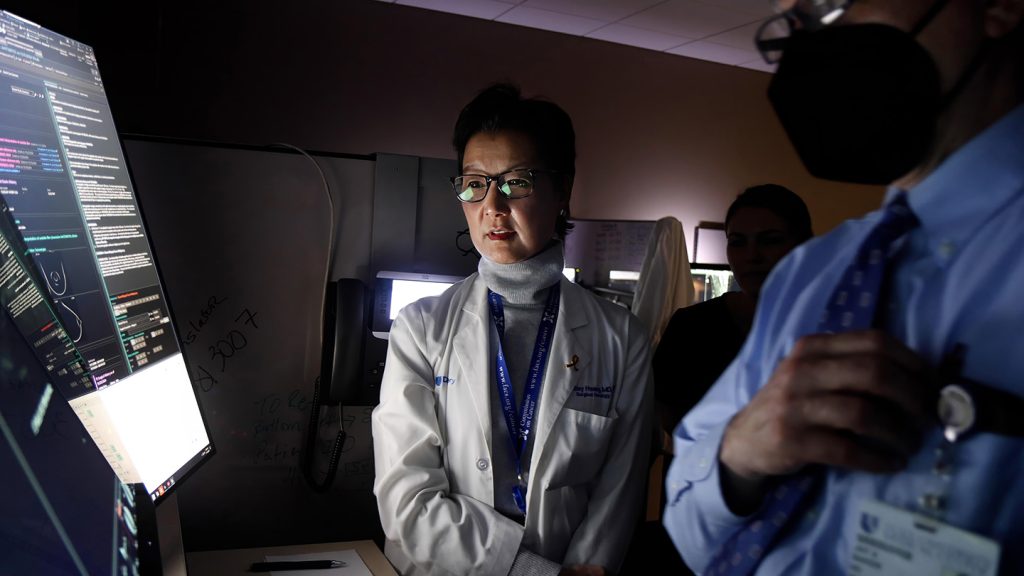
Ductal carcinoma in situ (DCIS), often referred to as Stage 0 breast cancer, presents a unique challenge in cancer management. While technically considered a noninvasive form of breast cancer, confined to the milk ducts, DCIS carries the potential to progress to invasive cancer. Traditionally, the standard approach has been surgical removal, aiming to eliminate the precancerous cells before they can spread. However, a recent study published in JAMA has sparked debate by suggesting that active monitoring might be a viable alternative for certain low-risk DCIS patients.
The study, involving 957 women aged 40 and older with low-risk DCIS, compared active monitoring with immediate surgery. Participants in the active monitoring group underwent mammograms every six months and most received hormone therapy. Surprisingly, after two years of follow-up, the rate of invasive breast cancer was lower in the monitoring group (3.1%) compared to the surgery group (8.7%). This intriguing finding suggests that for some women, delaying surgery doesn’t necessarily lead to a higher risk of cancer progression and may even offer advantages. The cancers detected in the monitoring group were not significantly larger or more likely to have spread compared to those discovered during surgery in the other group.
This study’s results challenge the prevailing notion that immediate surgery is always the best course of action for DCIS. Proponents of active monitoring argue that it allows women to avoid potentially unnecessary procedures, including surgery, radiation, and chemotherapy, for a condition that may never become life-threatening. It offers a less aggressive approach, allowing women to retain their breasts and minimize treatment-related side effects and emotional distress. By carefully selecting appropriate candidates based on low-risk characteristics, active monitoring could personalize treatment strategies and prioritize patient well-being.
However, the study is not without its limitations and has generated considerable discussion within the medical community. One primary concern is the short follow-up period of just two years. While initial results are promising, longer-term observation is crucial to fully understand the implications of delaying surgery. Cancer progression can be a slow process, and two years may not be sufficient to detect all cases of invasive cancer that may arise from DCIS. Critics argue that delaying surgery might increase the risk of larger tumors and subsequent spread to lymph nodes, potentially necessitating more aggressive treatment later on. A nuanced cost-benefit analysis considering the long-term risks and benefits of active monitoring is needed before it can be widely adopted.
Furthermore, the study’s focus on low-risk DCIS limits its generalizability. The participants had tumors with less aggressive features and hormone receptor positivity, making them responsive to hormone therapy. This specific selection criteria excludes a significant portion of DCIS patients with higher-risk factors, such as larger tumor size, comedo necrosis, or hormone receptor negativity. For these individuals, immediate surgical removal remains the recommended approach. Future research needs to explore whether active monitoring can be safely extended to other subgroups of DCIS patients.
Another significant point of contention revolves around patient preferences and decision-making. The women who volunteered for the study expressed a strong desire to avoid surgery, which might not be representative of the general DCIS population. Many women diagnosed with DCIS experience significant anxiety and prefer immediate removal to alleviate their concerns, even if the risk of progression is low. Shared decision-making between patients and their physicians is critical, ensuring that treatment choices align with individual preferences and values. Patients should be fully informed about the risks and benefits of both active monitoring and surgery, enabling them to make informed decisions that are consistent with their personal circumstances and emotional well-being.
The accompanying study published in JAMA Oncology sheds light on the quality of life experienced by women in both groups. Contrary to expectations, the study found no significant difference in worry levels between the active monitoring and surgery groups. This suggests that active monitoring, when deemed appropriate, doesn’t necessarily lead to increased anxiety and may be a psychologically acceptable option for some women. However, further research is needed to explore the long-term psychological impact of active monitoring, especially as it relates to the uncertainty surrounding potential cancer progression.
In conclusion, the recent JAMA study provides compelling preliminary evidence supporting active monitoring as a potential alternative to immediate surgery for select low-risk DCIS patients. However, the limited follow-up duration, focus on a specific subgroup, and the potential for selection bias underscore the need for cautious interpretation and further investigation. Longer-term studies encompassing a broader range of DCIS patients are essential to validate the safety and efficacy of active monitoring. Ultimately, the decision to pursue active monitoring or surgery should be made in close consultation with a healthcare professional, taking into account individual risk factors, patient preferences, and the potential long-term implications of each approach. Personalized treatment strategies that respect individual needs and values will optimize outcomes and promote the overall well-being of women facing the complex challenges of DCIS.